Circadian Rhythm Sleep Disorders
Expert Insights from Dr. Brooke Dulka, a medical writer and neuroscientist who received her Ph.D. in biological psychology from the University of Tennessee, and she is currently a postdoctoral researcher at the University of Wisconsin-Milwaukee where she studies the neurobiology of memory.
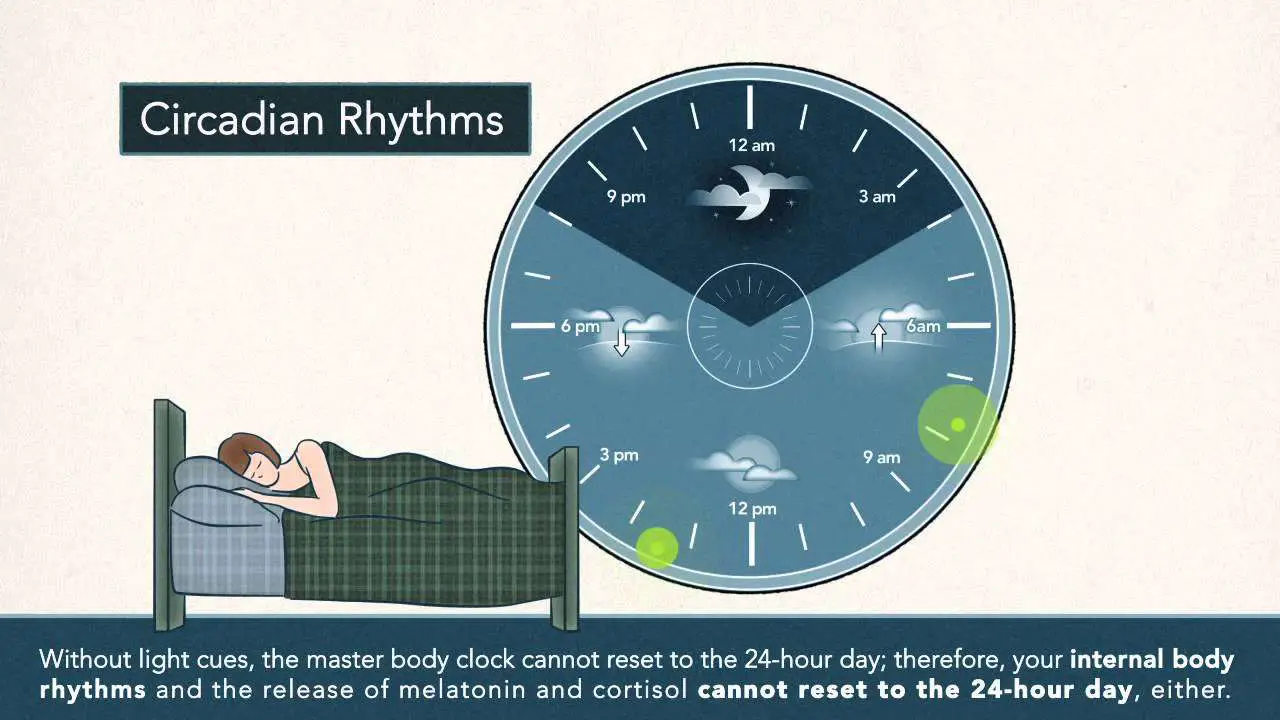
Circadian rhythm is our internal 24-hour clock. It cycles around in predictable patterns every day telling us when to sleep, when to wake up, when to eat, and so on. This master clock is operated by a group of neurons in the brain called the suprachiasmatic nucleus which takes cues our body sends when it senses changes in the environment.
For example, when we see the sun setting and night fall, sensors in our eyes send a message to the suprachiasmatic nucleus which triggers the production of melatonin, the hormone that makes us sleepy.
For most people, this process works like, well, clockwork. But some peoples internal clocks fall out of rhythm, and their sleep-wake cycle is disrupted. This can result in a circadian rhythm sleep disorder.
Are Narcolepsy Symptoms Different In Children
There is considerable overlap between narcolepsy symptoms in children and adults, but there are important differences as well.
In children, EDS is more likely to appear as restlessness or irritability, which may be interpreted as a behavior problem. At night, children with narcolepsy may sleep longer and have more active body movements during sleep.
Cataplexy is often more subtle in children, although it occurs in up to 80% of cases. It commonly involves the face rather than the body and may be perceived as a facial tic. Cataplexy in children may not be tied to an emotional response. Over time, cataplexy symptoms in children evolve to their more traditional form.
What Are The Symptoms Of Narcolepsy
The symptoms of narcolepsy can have notable effects during both daytime and night time. The most common symptoms include:
Although all people with narcolepsy have EDS, less than a quarter have all of these symptoms. In addition, the symptoms may not occur simultaneously. For example, its not uncommon for cataplexy to begin years after a person has started to have EDS.
You May Like: Best Mattress For 300 Pound Side Sleeper
What Objective Test Can Confirm Non
Hello. I’m 25M/NB, and I have autism, PTSD, exercise intolerance, fatigue, and some sort of sleep disorder. Possibly gender dysphoria, ME/CFS, and N24. I’m sighted.
I’m quite certain I have N24 because my bedtime gets later and later each day. I tracked my sleep and wake times for over a year and got the characteristic pattern. Because of my multiple impairments, I’ve never worked much and I’ve been forced to apply for disability. By law, SSA must use test results and clinical signs in determining someone to be disabled, hence my question.
I’ve taken a sleep study, and it came back normal. Now I have a follow-up appointment. I will advocate for a diagnosis of N24 and ask for testing. Is there an objective test that can confirm a N24 diagnosis, without relying on my self-report?
Conflict Of Interest Disclosures
Dr. Weaver has served as a consultant to Pfizer, Inc., for knowledge of molecular mechanisms of circadian rhythm regulation. Some work on melatonin receptor isolation and characterization was supported by a sponsored research agreement between S.M. Reppert and Bristol-Myers Squibb, via an institutional agreement through Massachusetts General Hospital.
Dr. Lockley was the principal investigator of three clinical trials of tasimelteon administration for the treatment of Non-24-Hour Sleep-Wake Disorder in the blind, sponsored by Vanda Pharmaceuticals. Inc., and has received an investigator-initiated research grant and two service agreements related to non-24-h rhythms in the blind from Vanda Pharmaceuticals, Inc., all via institutional agreements with the Brigham and Women’s Hospital. He has also received minor consulting fees from 15 investment firms discussing publicly-available information about the tasimelteon clinical trials. He has also received honoraria from MediCom Worldwide, Inc., for teaching in a CME course sponsored by Vanda Pharmaceuticals, Inc. for contributing text about non-24-h sleep-wake disorder for the National Sleep Foundation and textbook chapters published by Elsevier and in 2007 received authorship fees from Servier Inc., for writing a review of circadian rhythm disorders in the blind.
Steven W. Lockley, … Makoto Uchiyama, in, 2012
Don’t Miss: Difference Between P5 And P6 Sleep Number Bed
Behavioral Approaches To Treatment
Behavioral approaches are non-medical forms of therapy, and there are multiple ways that they can be incorporated into the daily habits of people with narcolepsy.
- Planning short naps: Because brief naps are refreshing for people with narcolepsy, budgeting time for naps during the day can reduce EDS. Accommodations at school or work may be necessary to make time for naps.
- Having healthy sleep hygiene: To combat poor sleep at night, people with narcolepsy can benefit from good sleep habits. Good sleep hygiene includes a consistent sleep schedule , a sleep environment with minimal distractions and disruptions, and limited use of electronic devices before bed.
- Avoiding alcohol and other sedatives: Any substance that contributes to sleepiness may worsen daytime narcolepsy symptoms.
- Driving with caution: People with narcolepsy should talk with the doctor about safe driving. Napping before driving and avoiding long or monotonous drives are examples of measures to improve safety.
- Eating a balanced diet: People with narcolepsy have a higher risk of obesity, which makes eating well an important part of their overall health.
- Exercising: Being active can help prevent obesity and may contribute to improved sleep at night.
- Seeking support: Support groups and mental health professionals can promote emotional health and counteract the risks of social withdrawal, depression, and anxiety in people with narcolepsy.
How To Treat Circadian Rhythm Sleep Disorders
Treatments used to treat your CRSD will depend on your specific condition and may include:
- Bright light therapy, using bright light at desired wake-up times, and darkness at desired sleep times.
- Chronotherapy, a process of gradually adjusting your bedtime until it reaches your desired bedtime to reset your circadian clock.
- Oral supplements like melatonin to induce sleepiness.
- Oral medications, like stimulants to promote wakefulness or hypnotics, to promote sleepiness.
- Lifestyle changes, such as sticking to a strict nap schedule and controlling your exposure to light, and cutting back on substances like caffeine or nicotine before bed.
- Sleep hygiene, such as improving your sleep environment.
Also Check: Associates In Sleep Medicine Orland Park
Causes And Risk Factors Of Non
Non-24-hour sleep-wake disorder is a disorder of the circadian rhythm that happens when the body’s internal clock is not synced with earth’s light and dark cycles of day and night. Affected individuals go to sleep later every night and wake up later the following day. Ultimately, the patient’s schedule for sleep goes all the way around the clock. For example, an affected individual may go to sleep at nine and wake up at nine in the morning, but the next night they won’t go to sleep until eleven at night. This means they wake up at eleven the next day. The delay is pushed back by a few hours each night until the individual is back to falling asleep and waking up at nine again. The circadian clock is a cluster of thousands of brain nerve cells that transmit signals throughout the body when it’s time to sleep or wake up.
Various causes and risk factors are associated with this disorder. Learn about them now.
What It Is Who Is Affected By It What Causes It And What Treatments Are Available
For most people, the body clock follows a 24-hour cycle known as the circadian rhythm. Sleep timing, appetite, and energy levels are all impacted by this circadian rhythm. A master clock in the brain called the suprachiasmatic nucleus controls circadian rhythm.
Most peoples innate body clock is actually slightly longer than 24 hours. However, the SCN enables us to stay synchronized to the 24-hour rhythm using cues from ambient light and other zeitgebers, or time-givers. Among other things, the SCN triggers sleep onset by signaling the release of the sleep hormone, melatonin, when it gets dark.
Non-24-hour sleep-wake disorder, formerly called free-running rhythm disorder or hypernychthemeral syndrome, refers to a condition in which the body clock becomes desynchronized from the environment.
Read Also: Sleep Number Bed Help With Snoring
Why Is It Important To Participate
Joining the Patient Registry for Blind Subjects with Sleep-Related Problems will help researchers better understand sleep-related problems in people who are blind, including investigation of potential therapeutics. The registry will help researchers identify and recruit patients who are eligible for participation in future clinical studies and to provide a forum for raising awareness about Non-24. Participants will have the chance to take part in a survey. The survey consists of questions regarding the degree of vision impairment and sleep problems that individuals may be experiencing. Patients enrolled in the registry will also have the option of receiving notification of upcoming research projects for which they may be eligible.
Conclusions And Future Directions
Circadian-based basic science developments continue to outpace clinical research pertaining to CRSWDs. Since publication of the prior Practice Parameters, relatively few new studies have emerged, although it is encouraging that investigations specifically oriented to the pediatric/adolescent and other special populations have been published. The major change with the present review is the use of the GRADE system of analysis. While more rigorous in many respects than the previously employed evidence-based assessment, derived data is designed to be more clinically relevant, as the GRADE system requires a combined consideration of strength of evidence, in conjunction with risk/benefit analyses and determination of patient values and preferences. As such, many previously endorsed practice recommendations have been negated, and numerous PICO questions remain unanswered. While this certainly points out the significant gaps with respect to the clinical CRSWD research , these updated Practice Parameters are intended to provide clinicians with heightened confidence in prescribing treatments and, equally importantly, they should serve as a roadmap for future studies that will propel higher quality, more sophisticated CRSWD therapies.
Don’t Miss: Sleep Number Split King Adjustable Bed Assembly
Internal Body Clock Issue
The internal clock of the human body is called the circadian clock. Non-24-hour sleep-wake disorder occurs when there is a problem with an individual’s internal rhythms. When light moves from the eyes to the brain, the internal body clock activates. If the patient is not completely blind, they may have issues with the mechanism of how light moves from their eyes to their brain. The individual will not have problems with vision, but their brain is not receiving the start-up trigger that it needs to tell the body it is time to go to sleep or wake up. The circadian clock should be synchronized with the physical environment of the patient by numerous light related and non-light related stimuli. The circadian rhythms in the hypothalamus manage many biological processes including body temperature, hormone secretion, cell-cycle regulation, feeding, glucose homeostasis, and the sleep-wake cycle. When there is an alteration in the timing of these physiologic rhythms, it causes internal desynchronization. This coordination loss of rhythms can have adverse consequences on the affected individual’s rest-activity cycles.
Uncover more risk factors and causes of non-24-hour sleep-wake disorder now.
Access To Unapproved Drugs
Governments worldwide have created provisions for granting access to drugs prior to approval for patients who have exhausted all alternative treatment options and do not match clinical trial entry criteria. Often grouped under the labels of compassionate use, , or named patient supply, these programs are governed by rules which vary by country defining access criteria, data collection, promotion, and control of drug distribution.
Within the United States, pre-approval demand is generally met through applications , or single-patient INDs. These mechanisms, which fall under the label of expanded access programs, provide access to drugs for groups of patients or individuals residing in the US. Outside the US, Named Patient Programs provide controlled, pre-approval access to drugs in response to requests by physicians on behalf of specific, or “named”, patients before those medicines are licensed in the patient’s home country. Through these programs, patients are able to access drugs in late-stage clinical trials or approved in other countries for a genuine, unmet medical need, before those drugs have been licensed in the patient’s home country.
The was established in November 2001 by Frank Burroughs in memory of his daughter, Abigail. The Alliance seeks broader availability of investigational drugs on behalf of terminally ill patients.
In 2013, was at the center of a high-profile debate regarding expanded access of cancer patients to experimental drugs.
Also Check: How To Sleep After Smoking Crystal
Delayed Sleep Phase Disorder
This type of circadian rhythm sleep disorder is the most common. It occurs when someone goes to sleep but wakes later more than two hours later than what is considered normal. People with DSP tend to be night owls, sometimes staying awake until 1 a.m. or later and waking up in the late morning or early afternoon.
This condition is more common in adolescents and young adults. There is some debate whether DSP is actually a sleep disorder among teens or if its just a normal but unexplained phase of the circadian rhythm development.
Symptoms
Delayed sleep phase disorder is hallmarked by feeling most alert in the evening and an inability to fall asleep at the desired time. Individuals with this disorder have an overall sleeping and waking schedule that is pushed back by at least two hours. They generally go to bed between 1-4 AM. and wake between 8-11 AM. The inability to fall asleep is considered a form of insomnia, but when coupled with an inability to wake up it is considered a sleep disorder. For people with delayed sleep phase disorder, the challenge with sleep is on both ends and the entire schedule is pushed back.
When is being a night owl a problem? When it interferes with work or school, or when it is evident it is causing depression or other behavioral health issues. It then ceases to be just a syndrome and is classified as a disorder.
Causes
Background The Molecular Clock
The ability to anticipate predictable environmental changes and adapt behavioral responses to daily or seasonal variations is a highly conserved biological program among various species, from single cell organisms to more complex life forms, such as insects, rodents, birds, and humans .
The phenomenons underlying principle, a genetically encoded molecular clock, basically consists of positive and negative feedback mechanisms of DNA translation: the dimerization of the transcription factor CLOCK with BMAL1/2 or NPAS2 initiates the expression of the clock proteins PERIOD and CRYPTOCHROME , which accumulate and inhibit CLOCK:BMAL1/2 activity, blocking their own expression and therefore closing the cycle . These molecular loops intrinsically generate a circadian rhythm , which is then directly or indirectly translated into behaviors, such as locomotion and feeding or sleep-wake cycles, according to environmental settings. While the period length remains relatively stable, the phase is influenced and reset by external cues, with the most important zeitgeber being the 24-h LD cycle .
Read Also: Sit And Sleep Torrance California
How Are Circadian Rhythm Sleep Disorders Diagnosed
CRSDs are usually only diagnosed when the phase advance or phase delay differs from the norm by at least two hours . In some cases of a CRSD, the phase shifts may be three to five hours or more.
You will need to see a doctor or a sleep specialist to be diagnosed and ultimately treated for a circadian rhythm sleep disorder. Your doctor will probably ask you to record when and how well you sleep over a period of time. They may also have you wear a small device called an actigraphy on your wrist to record your movements so they can better understand your sleep cycle.
Recommendations Are As Follows
ASWPD
5.1.4a The TF suggests that clinicians treat adult ASWPD patients with evening light therapy .
DSWPD
5.2.6.1a The TF suggests that clinicians treat DSWPD in adults with and without depression with strategically timed melatonin .
5.2.6.2.1a The TF suggests that clinicians treat children and adolescents with DSWPD with strategically timed melatonin .
5.2.6.2.2a The TF suggests that clinicians treat children and adolescents with DSWPD comorbid with psychiatric conditions with strategically timed melatonin .
5.2.9.2a The TF suggests that clinicians treat children and adolescents with DSWPD with post-awakening light therapy in conjunction with behavioral treatments .
N24SWD
5.3.6.1a The TF suggests that clinicians use strategically timed melatonin for the treatment of N24SWD in blind adults .
ISWRD
5.4.4a The TF suggests that clinicians treat ISWRD in elderly patients with dementia with light therapy .
5.4.5a The TF recommends that clinicians avoid the use of sleep-promoting medications to treat demented elderly patients with ISWRD .
5.4.6.1a The TF suggests that clinicians avoid the use of melatonin as a treatment for ISWRD in older people with dementia .
5.4.6.2a The TF suggests that clinicians use strategically timed melatonin as a treatment for ISWRD in children/ adolescents with neurologic disorders .
Don’t Miss: Sleep Number Bed Labor Day Sale
What Are Circadian Rhythm Sleep Disorders
Circadian rhythm sleep disorders are a family of related sleep disorders, all characterized by an inability to sleep and/or wake at appropriate times due to the dictates of the individuals biological or circadian clock.
People with a circadian rhythm sleep disorder attempt to sleep at an abnormal time in their circadian cycle. Its like having jet lag all the time. Usually, the sleep is of normal quality, and even its quantity would be usually sufficient if the person were allowed to start and finish their sleep at the times dictated by their body clocks. But often this does not fit in with the schedule for normal work, school, or social needs.
How You Can Help Non
New research studies may lead to better understanding of Non-24 in children who are totally blind, and researchers are eager to better understand Non-24 and circadian rhythm problems in children who are totally blind. To that end, clinical studies will be conducted specifically in children and adolescents to determine whether a certain oral compound is safe and effective in treating Non-24 in the pediatric population.
Don’t Miss: Dr Barbara Sturm Sleep Food