Obstructive Vs Central Sleep Apnea: Key Differences And Treatment Options
Sleep apnea is a common sleep disorder that affects thousands of individuals. With this condition, you have an interruption in your breathing while sleeping that occurs through repetitive pauses, referred to as apneic events. There are several types of sleep apnea, but two prominent types include obstructive sleep apnea and central sleep apnea.
As a sleep technologist, its important for you to know the key differences between central and obstructive apnea so you know how to best treat your patients who may have one or the other disorder.
What Constitutes Sleep Apnea
When addressing the topic of how many people have sleep apnea, its vital to include what constitutes sleep apnea.
First, sleep apnea is a common sleep disorder that results in shallow breathing or causes someone to stop breathing for a few seconds to a few minutes.
This can occur more than 30 times per hour. When regular breathing begins again, the sufferer may make a choking or snorting sound.
One common misunderstanding about sleep apnea is that everyone with this disorder snores.
Not everyone snores if they suffer from sleep apnea. However, people with sleep apnea tend to snore loudly if they do snore.
What Are The Risk Factors Of Sleep Apnea
The most common type of sleep apnea is reportedly obstructive sleep apnea, which we will address later in this article.
The highest risk factors for sleep apnea include being overweight, family history of the condition, or being male.
Since how many people have sleep apnea isnt exclusive to obesity, gender, or genetics, some outliers may include children with enlarged adenoids or tonsils.
Sleep apnea is not a cookie cutter sleep disorder.
Here is a list of some other risk factors you should know.
- Getting older
- Recent high altitude ascents
Also Check: Sleep Number Spring Hill Tn
What Can Happen If Sleep Apnea Is Left Untreated
There are some complications that can occur if sleep apnea is left untreated. Sleep apnea has been linked to the increase in risk factors for the following:
- Asthma symptoms
- Inability to focus, memory issues, and other forms of cognitive issues
Another common misconception about sleep apnea, regardless of the type, is that its harmless.
It may not always cause complications like the above, but the potential is there, especially if one has other health issues or is elderly.
The links between complications and sleep apnea are still unclear, but are often seen as per reports by medical doctors and researchers.
Therefore, no matter what, anyone with sleep apnea should seek advice from a medical professional to not only treat the condition, but to find out if there is an underlying medical problem.
How Many People Have Sleep Apnea In 2022
Data from 2021 reveals that approximately 12%, or around 30 million American adults suffer from sleep apnea.
Worldwide, its estimated that about 936 million people have sleep apnea.
If you notice that your child, spouse, or other loved one is temporarily not breathing and then starts up suddenly after a loud snore or snort, its wise to go get a diagnosis from a doctor since this condition can result in long-term health problems if left untreated.
As we will do throughout this article, its better to see a doctor if you have the symptoms of this sleep disorder than to ignore sleep apnea.
Also Check: Sleep Number Mattress On A Platform Bed
Identifying Complex Sas Patients Using Psg Data: Complex Sas Phenotypic Features
Two types of complex disease are described: hypocapnic and hyper-capnic . Gilmartin et al7 reported several identifiable variables linked to the hypocapnic variety .
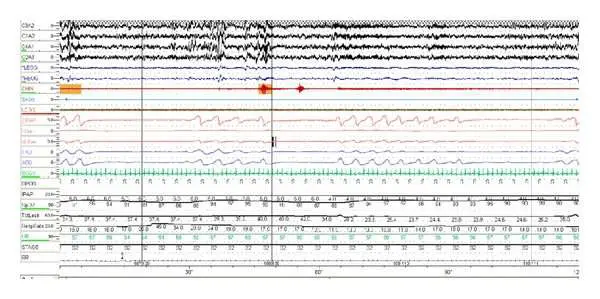
Complex SAS patients present with mixed types of apneas rather than pure obstructive or central apneas on the PSG.7 The hypopneas are obstructive but oscillate similar to periodic breathing-waxing and waning symmetrically. From the baseline PSG data, the total apnea hypopnea index was statistically different between the complex SAS, CSA and OSA groups with the OSA group having the lowest AHI. Complex SAS patients also had a statistically significant higher nonrapid eye movement sleep obstructive AHI than did CSA and OSA patients and total obstructive AHI .1 . It is not known what minimum number of mixed apneas indicate complex SAS in SDB patients, but it is possible that recognition of one mixed apnea during the automated or manual scoring of the PSG breathing events may point toward the existence of complex SAS.
The nasal pressure cannula airflow signal showing variations relative to the upper airway obstruction that are intermixed with periodic breathing respiratory effort suggest the presence of complex SAS. These variations are better observed by increasing the epoch size from 30 to 90 or 120 seconds.
Specific Intervention For Tecsa: Is It Necessary
As some authors reported, TECSA may be a self-limited disorder in some patients. Some central respiratory events are transient and could spontaneously resolve over time with ongoing treatment with CPAP therapy. In a case report, Mohan et al reported that spontaneous resolution of MAD-emergent CSA was seen more than 1 year after the maintenance of MAD treatment in a patient with moderate OSA who refused PAP therapy the authors suggested that the key to the resolution of central respiratory events should be strict adherence to effective therapy. However, central apneas still persist in some patients even with regular CPAP therapy. Hence, there is still some controversy about the optimal method for treating TECSA.
You May Like: How To Lose Weight Fast While Sleeping
Polysomnographic Characteristics A Priori
Based on the diagnostic PSG to establish OSAS, it is not possible to predict whether someone will present with CompSAS. Some evidence has been reported that CompSAS patients might have a higher CAI at diagnosis than OSAS patients , but this could not be confirmed by others . One study reported a significantly higher CAI in non-rapid eye movement sleep and in supine position, but the differences were small and not clinically relevant . During CPAP titration, CompSAS patients present central apnoeas most often during NREM sleep, and certainly much fewer or no apnoeas during REM sleep . A higher arousal index was reported in CompSAS in one study , but was not confirmed in other studies .
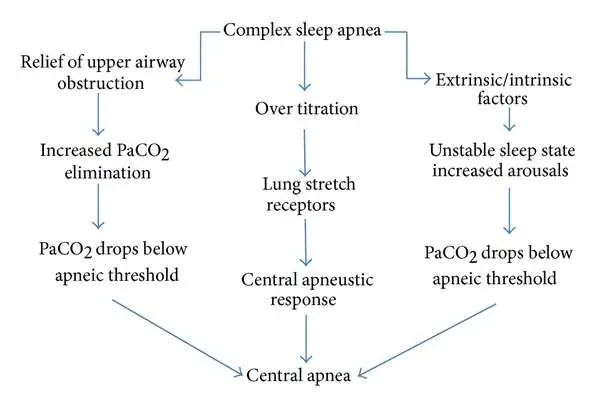
Activation Of Lung Stretch Receptors
Expansion of lung volumes induced by over-titration of CPAP may lead to activation of stretch receptors in the lungs the receptors then send signals via the vagal nerve fibers to the respiratory center, which then inhibits the central respiratory output. Consequently, an interruption of inspiration will occur. This mechanism can also protect the lungs against overexpansion.
Don’t Miss: What Is The Best Type Of Mattress To Sleep On
First What All Types Of Sleep Apnea Have In Common
Because these awakenings are typically very brief, the person with sleep apnea may not even be aware that they are experiencing interrupted sleep. But the episodes can wreak havoc on the sleep cycle and prevent the person with sleep apnea from reaching the deep, restful phases of sleep. And thats why people who have sleep apnea can experience significant exhaustion and drowsiness the next day, despite getting what they thought was a full night of sleep.
What Increases The Risk Of Complex Sleep Apnea
Atrial fibrillation, family history of complex/central sleep apnea, heart failure, male sex, renal failure, and stroke are factors that are associated with complex sleep apnea. The majority of complex apnea patients probably have a genetic risk, just as the amount of central apnea seen in individuals going to high altitude varies substantially even with the same degree of exposure. The genes controlling sensing of O2 and CO2 could alter the control pathways at many sites as the breathing control system is very elaborate.
Also Check: Why Did I Pee In My Sleep Last Night
Risk Factors And Clinical Characteristics
Certain risk factors, including demographic data, clinical information, and polysomnographic characteristics, are associated with a higher prevalence of TECSA .2]. Some studies identified several clinical risk factors for TECSA in OSA patients. As these studies reported, older age, male, lower body mass index, comorbid conditions , medications , certain polysomnographic parameters at the time of diagnostic polysomnography study , and titration factors in their titration studies) were associated with a higher prevalence of TECSA in OSA patients than those in matched control subjects. Lei F et al reported that higher baseline mixed sleep apnea, especially in non-rapid eye movement sleep, was related to a higher incidence of TECSA in OSA patients. Herkenrath S et al compared mixed apnea metrics during diagnostic PSG in OSA patients with or without TECSA, and found that those with TECSA had longer apneic duration, more frequent arousals, and shorter ventilatory duration, consistent with higher ventilatory control instability. However, there is still no consensus on the risk factors for TECSA, and the same risk factors are not always identified in the different studies.
Sleep Apnea Home Treatment
As previously mentioned, lifestyle changes can be used to help treat sleep apnea, particularly the mild variants. Lifestyle recommendations from a doctor can include:
- Avoiding alcohol and sleeping pills Many people who have issues with sleep have a tendency to turn to either or both of those things. Alcohol might make it easier for you to get to sleep, but it disrupts your sleep cycles and causes excess muscle relaxation which can make your sleep apnea worse.
- Changing sleep positions Staying off your back can play a major role in breathing more easily. If you have a tendency to roll on to your back at night, there are many pillows available to keep you on your side. You can even try placing a pair of tennis balls in a tube sock then pinning them to the backside of your pajama shirt.
- Losing weight Roughly half of the people that deal with sleep apnea are overweight. Thats because extra weight will likely lead to extra tissue in the throat. In turn, breathing will be harder to do. Healthy, sustainable weight loss can be a tool to reduce the severity of sleep apnea.
- Quitting smoking Smoking leads to upper airway swelling, which can worsen sleep apnea. It can also lead to snoring or, if a person already snores, it will worsen.
- Treating allergies Airways tissues swell when nasal allergies are at play. It makes the pathway more narrow, leading to breathing problems. Work with your physician to stay on top of those allergy symptoms, especially when going to bed.
You May Like: Will Treating Sleep Apnea Help Me Lose Weight
How Asv Machines Work
Whenever the ASV machine detects abnormalities in breathing, it intervenes with just enough support to maintain the patient’s breathing at 90% of what had been normal for that patient prior to the abrupt change in breathing. When the patient’s breathing problem ends, the machine re-adjusts itself to the patient’s normal breathing pattern.
When the patient’s breathing is stable, ASV provides just enough pressure support to provide an approximate 50% reduction in the work of breathing for the patient, therefore making the therapy much more comfortable for the patient.
How Is Central Sleep Apnea Diagnosed
A definitive diagnosis of CSA is made using an in-lab polysomnography, which is a detailed sleep study that measures breathing, respiratory effort, electrocardiogram, heart rate, oxygen, eye movement activity, muscle activity, and electrical activity of the brain during an overnight stay in a sleep clinic.
Because central sleep apnea can be tied to several health problems, a healthcare provider may also recommend other tests, such as a brain scan or an echocardiogram of the heart to determine the underlying cause.
Anyone who has noticed potential symptoms of central sleep apnea should speak with a doctor who can review their situation and determine if any diagnostic testing is appropriate.
Read Also: Sleep Number Return Shipping Cost
A Physician’s Personal History Of Complex Sleep Apnea
I coined the term complex sleep apnea in 2004 and a year earlier had described a NREM-dominant obstructive sleep apnea syndrome. However, since early in my sleep medicine training days in the mid 1990’s, I was puzzled by the subset of patients who appeared to have obstructive sleep apnea but were difficulty to treat properly in the sleep laboratory. In particular, they persistently stated an inability to use, or intolerance to, positive airway pressure, despite their honest efforts to use it.
In those days the type of breathing monitoring now available in positive pressure devices did not exist, so we were largely blind to what happened during patients’ nightly use. I also remember noting that bilevel positive airway pressure was often resulted in worse responses than continuous positive airway pressure . In fact, in patients with NREM dominant sleep apnea, auto CPAPs seemed to chase changing breathing patterns with pressures that went up and down during sleep, resulting in even poorer results than use of fixed CPAP.
Central Sleep Apnea Happens When The Brain Is Involved
Central sleep apnea is less common than obstructive sleep apnea. It can also be trickier to diagnose and treat. Unlike obstructive sleep apnea, which is caused by a mechanical problem that blocks the airway, central sleep apnea occurs because the brain is not sending the proper messages to the muscles that control breathing. Central sleep apnea is caused by a neurological reason, explains Dr. Capasso.
Also Check: Does Smoking A Cigarette Help You Sleep
Central Sleep Apnea Risk Factors
Anyone could have any of the types of sleep apnea. Central sleep apnea is more common among older people, especially those over 65. They may have health conditions or sleep patterns that make them more likely to get CSA.
Men are at higher risk of both central and obstructive sleep apnea.
Conditions that may be linked to central sleep apnea include:
- Avoid alcohol and sleeping pills, which make your airway more likely to collapse while you sleep.
- Sleep on your side instead of on your back.
- Use nasal sprays or breathing strips to keep air flowing if you have sinus problems or nasal congestion.
- Get plenty of sleep.
Continuous positive airway pressure can help people with all kinds of sleep apnea, especially CSA caused by heart failure.
A CPAP machine forces a constant stream of air into your nose and mouth through a mask you wear while you sleep. The air pressure is just enough to keep your upper airway tissues from collapsing and blocking your breathing. If you have trouble with CPAP, you might try similar devices called adaptive servo-ventilation and bilevel positive airway pressure .
A device called the Remede System can help with moderate to severe central sleep apnea. Your doctor implants a small machine under the skin in your upper chest. It helps trigger the nerve that moves your diaphragm when you breathe. It also monitors your respiratory signals while you sleep and helps restore regular breathing patterns.
Continued
Complex Sleep Apnea Syndrome
Accepted for publication 15 May 2013
3 July 2013Volume 2013:7 Pages 633641
This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at and incorporate the Creative Commons Attribution – Non Commercial License.By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Don’t Miss: Sleep Number Twin Adjustable Base
What Is Complex Sleep Apnea Syndrome
The most common form of sleep apnea is obstructive sleep apnea, in which a person has difficulty breathing regularly at night due to an obstruction in the airway. Obstructive sleep apnea can be treated in a variety of ways, including lifestyle changes, positional therapy, oral devices, continuous positive air pressure devices, and sleep apnea surgery.
The second most common form of sleep apnea is central sleep apnea, in which a person has difficulty breathing because of a neurological issue unrelated to their airway. While the symptoms of CSA are the same as OSA, the causes are different and include: Parkinsons disease, certain medications, and heart disease.
Complex sleep apnea syndrome is a combination of obstructive sleep apnea and central sleep apnea. It is often discovered after a patients OSA is treated when symptoms of sleep apnea remain even after the airway is cleared. While some patients may simply have both common types of the disease, some doctors believe that complex sleep apnea only emerges after OSA is treated. A Mayo Clinic study found that an estimated 15 percent of OSA patients actually suffer from some form of complex sleep apnea.
What You Should Know About Treatments For Sleep Apnea

- Sleep Apnea
Sleep apnea is a serious sleep disorder that causes you to stop and start breathing repeatedly when you sleep. It can lead to fatigue even after youve had a full nights rest. There are several types the main ones include:
Central sleep apnea This happens when the wrong signals are sent by the brain to the muscles that are responsible for breathing.
Complex sleep apnea syndrome Another term for this is treatment-emergent central sleep apnea. It happens when people have a combination of central sleep apnea and obstructive sleep apnea.
Obstructive sleep apnea This is a common type. It happens when throat muscles relax and block your airway.
Also Check: Sleep Number Bed Frederick Md
What Are The Available Treatments For Complex Sleep Apnea
The only FDA-approved treatment is adaptive servo-ventilation . ResMed and Philips-Respironics have devices approved world-wide, and Weinmann has a device in Europe. These devices track breathing rhythm and create air pressure rhythms equal and opposite to the patients. They are at times very useful and effective, but at times the rhythm does not properly match and patients cannot tolerate the pressure fluctuations. The ResMed device was recently shown to worsen outcomes in patients with a certain type of severe heart failure. Interested readers can search the Internet with the keywords SERVE-HF and ResMed to find more information. One useful link is
If you use one of these devices, it is important that you discuss the benefits and risks with your physician. These are powerful devices that need to be used with care. All other treatment options are off-label and must be used only by physicians after a careful risk/benefit discussion. In my experience, oxygen is frequently tried, but rarely provides a high level of benefit. I have had some success combining an oral appliance with acetazolamide.