Upper Airway Stimulation Therapy
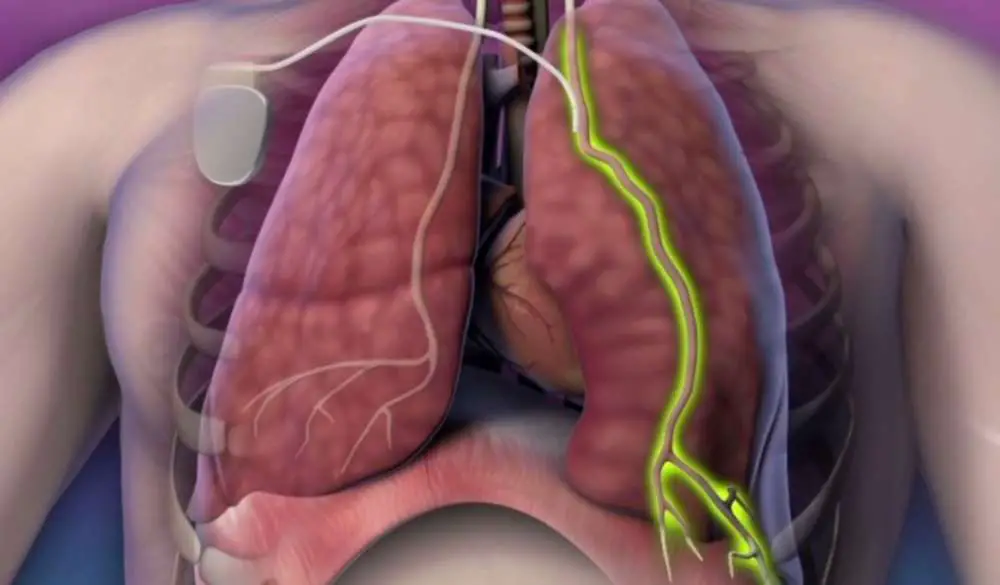
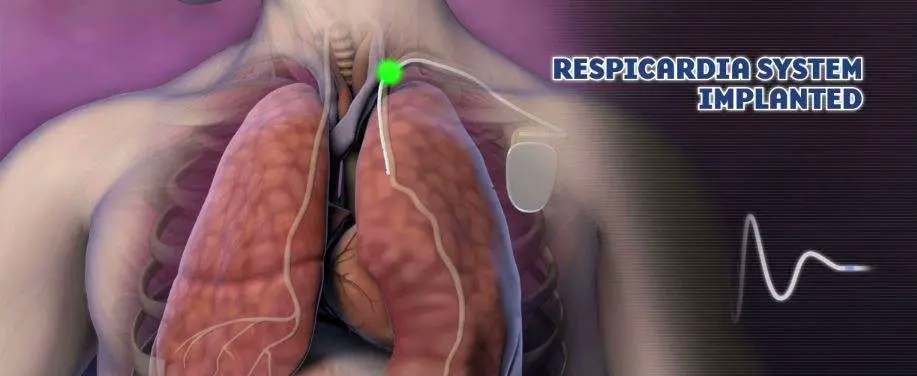
Upper airway stimulation involves an outpatient procedure to implant a device that monitors your breathing while you sleep. The device stimulates the hypoglossal nerve, which controls your tongues movements, pushing it out of the way to keep the airway open.
To be eligible, patients must have moderate to severe sleep apnea that cannot tolerate CPAP or oral appliance. They also must be at least 22 years old and not significantly overweight. Patients will have to meet with a surgeon to see if this procedure is an option for them. Patients can expect to have a sleep study before and after the procedure.
Before Trying Surgery For Sleep Apnea
Surgery is not for everyone, and it’s not always an easy fix solution for treating OSA. As you’ll discover on this page, surgery for sleep apnea has low rates of success. And success in surgery doesn’t always mean you are completely treated.
You should seriously consider trying a couple of non-surgical options before choosing surgery, such as:
Even doctors have sometimes difficulties to recommend which treatment is the best for you. Some surgeries for sleep apnea can have serious side effects, worsening the severity of the syndrome and affecting the treatment with other options available.
For example, after UPPP surgery patients can have problems to use the CPAP machine, even if its necessary. However, nasal surgery can help you tremendously to use CPAP with success, mostly if you have nasal congestion, enlarged turbinates or deviated septum.
Bottom line… Consider trying nonsurgical or conservative options to treat sleep apnea, before undergoing any surgery.
What You Need To Know About Sleep Apnea And Surgery
If you are contemplating any medical or dental procedures or surgery in the future, the following information is provided to assist you.
While sleep apnea has become a recognized medical condition within the medical community, one shouldnt assume that all healthcare professionals are aware of sleep apnea. It is the responsibility of any patient with a sleep disorder to make it known to their doctor, nurse, therapist, dentist and anyone involved in their medical care.
The preoperative conference with a member of the anesthesia department is an important time to get to know your anesthesiologist and to exchange the necessary information that will make the up and coming surgery a complete success. Always indicate to this member of the surgical team that you have sleep apnea and are using a CPAP device. Inform them of your prescribed device pressure. Ask the surgeon and anesthesiologist if it is appropriate or required to bring your CPAP with you to the hospital on the day of your surgery. Some surgery centers and hospitals prefer to use their own devices but they will need to know your prescribed pressure.
Following successful surgery and during your stay in the recovery room, it might be necessary to use CPAP, since your upper airway is still under the influence of sedating drugs and may be acting like you are asleep. During this transition from anesthesia to wakefulness, the use of CPAP can provide normal breathing until you are totally awake and alert.
Also Check: Sleep Number Wichita Falls Tx
Central Sleep Apnea Diagnosis
A central sleep apnea diagnosis can be completed by licensed physicians. The first step in a central sleep apnea diagnosis requires an examination, which generally includes the individual staying overnight in a sleep laboratory to receive a sleep study, or polysomnography, administered by a technician.
Periods of breathing cessation are measured in frequency during the sleep study, which will allow the technician to help determine what type of sleep apnea is present.In central sleep apnea, the interruption in breathing is associated with physically being unable to restart the cycle. A polysomnogram will show the relation between the cessation of airflow through the nose and mouth, as well as the absence of muscle movement in the rib cage and abdominal area.
Since central sleep apnea is frequently associated with heart, lung, or kidney diseases, there are other tests that are done with polysomnography, including:
- Lung function tests
If You Are Able To Perform Uppp Surgery You May Be At Risk Of Some Complications Including:

The soft palate and throat muscles may not work properly.
If antibiotics are not used before the operation, your throat may become infected.
You may have trouble swallowing.
You may feel fluid gushing from your mouth or nose.
You may not be able to smell it.
Having surgery to help you sleep better is not guaranteed. You may still experience sleep apnea episodes again.
Even using CPAP after surgery will not be as effective.
Recommended Reading: Who Sells Sleep Science Mattresses
Are There Other Treatments For Sleep Apnea
The first-line treatment for sleep apnea is continuous positive airway pressure . CPAP involves a person wearing a mask over their mouth and nose that is connected to a machine. The machine delivers a constant flow of air to a persons airways to help keep them open.
Doctors rarely recommend surgery to treat sleep apnea. A person may improve their sleep apnea in the following ways :
- making lifestyle changes, such as maintaining a healthy weight, limiting alcohol, stopping smoking, staying active, and eating a healthy diet
- using oral devices to open the mouth wider
- doing exercises for the mouth and jaw area
A person should talk with a doctor about their expectations following the procedure. Most of the procedures have a high level of success, though not everyone will see improvement following surgery.
If one surgical procedure does not work, a persons doctor will likely recommend additional treatments.
Anterior Inferior Mandibular Osteotomy
This procedure divides your chin bone into two parts, allowing your tongue to move forward. This helps open up your airway while stabilizing your jaw and mouth. This procedure has a shorter recovery time than others, but its usually less effective. Your doctor might also suggest doing this procedure in conjunction with another type of surgery.
Recommended Reading: Sleep Number Store Omaha Ne
Central Sleep Apnea And Sleep Related Hypoventilation/hypoxemic Syndromes
Central sleep apnea and sleep related hypoventilation/hypoxemic syndromes are sleep related respiratory conditions.
CSA occurs when you repeatedly stop breathing during sleep because your brain does not cue your body to breathe. This differs fromobstructive sleep apnea since in central sleep apnea, there is no breathing effort because there is no drive to breathe. In its primary form, CSA is the result of instability of the breathing control system as the individual transitions from wakefulness to sleep.
Sleep related hypoventilation/hypoxemic syndromes may be the result of a decreased response to low oxygen or high carbon dioxide during wakefulness and sleep and are characterized by frequent episodes of shallow breathing lasting longer than 10 seconds during sleep.
Issues With Respiratory Regulation
Another central sleep apnea cause is an issue with respiratory regulation. The brain and heart normally work together to keep a balanced level of oxygen and carbon dioxide in the bloodstream. However, the heart and brain may differ in what each organ considers normal inhalation and exhalation cycles.
Central sleep apnea causes the neurological centers in the brain that are responsible for breathing cycles to fail to react fast enough to keep the respiratory rate even and unlabored. This causes the respiratory rate to fluctuate between central sleep apnea and hypopnea episodes throughout the night.
During the breathing pauses, the individual makes no efforts to start breathing again, the chest does not move, and the muscles do not relax or contract. Individuals will wake up and not be able to immediately start breathing again, leading to a feeling of panic and cognitive dysfunction. These symptoms are associated with excess carbon dioxide levels in the blood.
Don’t Miss: Why Do Men Get An Erection While Sleeping
Bilevel Positive Airway Pressure
Bilevel positive airway pressure is effective for treating patients with hypercapnic central sleep apnea . The inspiratory positive airway pressure is higher than the expiratory positive airway pressure . A high IPAP-to-EPAP differential provides breath-by-breath pressure support to augment ventilation. In addition to reinforcing the spontaneous breaths, patients with central sleep apnea may require additional breaths set as a back-up rate, especially when the central apneas are long. Patients with high-pressure requirements may benefit by elevation of the head end to 45-60°, which often dramatically decreases their pressure requirements.
Pressure-cycled BIPAP is usually adequate. Volume-cycled ventilators are rarely necessary and have their own limitations in terms of inability to adjust for high leaks, humidification, and expense.
Some patients with nonhypercapnic central sleep apnea, such as CSB-CSA, and primary central sleep apnea have been shown to benefit from BIPAP. Because BIPAP can be used with a back-up rate, it is beneficial in patients with long apneas. However, BIPAP, especially when used with a high IPAP-to-EPAP differential, has the potential to worsen central sleep apnea by lowering the PaCO2. BIPAP has been used to treat patients with heart failure and CSB-CSA with variable results and further studies are needed to better assess the role of BIPAP treatment in this group of patients.
Continuous Positive Airway Pressure Machines
In many cases of sleep apnea, doctors will suggest using a continuous positive airway pressure machine as a first line of treatment.
CPAP machines move air through a mask and into the persons airways. This can help reduce the likelihood of sleep apnea, as the force of the air helps keep the airways open and air moving through them.
That said, CPAP machines may not be effective in people with central sleep apnea. A study in the Journal of the American College of Cardiology notes that CPAP is only effective in about 50% of people with central sleep apnea.
If CPAP does not improve symptoms, it is important to seek an alternative treatment option.
Don’t Miss: Sleep Number High Point Nc
Risk Factors And Related Conditions
Central sleep apnea can affect patients of all ages. However, there are statistical factors that coincide with a potentially higher risk of patients developing the condition, including:
- Being male, as they are more likely to develop the condition than females
- Older age, especially adults over 65 years of age
- Having a heart condition, such as an irregular heartbeat
- Opioid use in any capacity
- Suffering from a brainstem lesion, stroke, or brain tumor, any of which can potentially impair the ability to regulating breathing
- Use of a continuous positive airway pressure machine, which is known as treatment-emergent central sleep apnea
Csa Due To Medication
Drugs in common use for pain control include morphine, fentanyl and methadone. Patients on high doses of these medications may have a slow sleeping respiratory rate. They may develop long obstructive apnoeas. Ataxic breathing is commonly observed with variation in respiratory rate and tidal volume. Relatively few arousals are noted and stage N3 can be increased. Periodic breathing and intermittent central apnoeas are seen and these may even occur in stage N3. Treatment emergent central apnoeas are also common even if the diagnostic study might have shown mainly obstructive events. Reduction in opiate dose is a logical first step if this were possible. Patients with mostly obstructive events respond to CPAP but then central apnoeas may emerge or persist . Javaheri et al. reported on ASV being effective treatment for both central and obstructive apnoea in opiate induced complex SA . It is essential to increase EPAP sufficiently to eliminate upper airway obstructive events in these situations.
Don’t Miss: Sleep Number Inner Circle Rewards
How Is Central Sleep Apnea Treated
Treatment for central sleep apnea must be conducted under the care of your physician. There are several options for managing the effects of central sleep apnea that physicians will often suggest. These include:
- A continuous positive airway pressure machine that provides enough pressure to keep the upper airway open via a mask
- Diaphragm pacing, a minimally invasive process that stimulates the phrenic nerve so that the patient can breathe more naturally
Specific Intervention For Tecsa: Is It Necessary
As some authors reported, TECSA may be a self-limited disorder in some patients. Some central respiratory events are transient and could spontaneously resolve over time with ongoing treatment with CPAP therapy. In a case report, Mohan et al reported that spontaneous resolution of MAD-emergent CSA was seen more than 1 year after the maintenance of MAD treatment in a patient with moderate OSA who refused PAP therapy the authors suggested that the key to the resolution of central respiratory events should be strict adherence to effective therapy. However, central apneas still persist in some patients even with regular CPAP therapy. Hence, there is still some controversy about the optimal method for treating TECSA.
Also Check: Sleep Number Store Franklin Tn
What Are The Different Types Of Central Sleep Apnea
Central sleep apnea is divided into two categories, and each of the categories has its subtypes.
The first category we will walk you through is the hypoventilation type. In this type of central sleep apnea, the brain fails to effectively send signals to the respiratory muscle to initiate breathing. Often, carbon dioxide builds up in these cases. Hypoventilation-type of central sleep apnea includes the following subtypes:
- Narcotic-Induced Central Sleep Apnea: In this type of central sleep apnea, the use of narcotics, such as opioids, diminishes the brains ability to properly initiate and regulate breathing.
- Central Sleep Apnea Related to a Medical Condition: This type of central sleep apnea often occurs as a result of a stroke, tumor, or trauma affecting the brain. Typically, the brain stem, a part of the brain that helps control breathing, is affected.
Related Reading
- Congenital Central Hypoventilation Syndrome : CCHS is a very rare genetic condition that most often affects newborns or very young children. There is a lack of signal to breathe during wakefulness and sleep
- Central Sleep Apnea Due to Neuromuscular Disease: Typically seen in amyotrophic lateral sclerosis or multiple sclerosis, central sleep apnea emerges due to extreme weakness in the respiratory muscles.
Surgeries Performed By An Ent Surgeon
Trans Oral Robotic Surgery enables a 3-D image that gives the surgeon a clear view of the operative field and the ability to safely remove obstructive tissue from behind the tongue. As part of the TORS procedure, the epiglottis may be trimmed, as some patients will experience obstruction due to the epiglottis falling into the airway during sleep.
Inspire Hypoglossal Nerve Stimulator: A backward collapse of the tongue, diagnosed via a nasal endoscopy, can be treated using the Inspire Hypoglossal Nerve Stimulator. This consists of a breathing sensor and a stimulation lead, powered by a small battery. Implanted during a short outpatient procedure, Inspire therapy continuously monitors breathing while the patient sleeps. The system delivers mild stimulation to key airway muscles, and gently moves the tongue and other soft tissues out of the airway to enable breathing during sleep.
Inspire Hypoglossal Nerve Stimulator
Uvulopalatopharyngoplasty or UP3 is a procedure designed to open the throat to allow improved breathing in patients with OSA. During this procedure, excess tissue in the throat is removed to widen the airway and allow air to move through the throat more easily. This reduces snoring and may be effective in select mild to moderate cases of OSA. The procedure is often combined with tonsillectomy and requires a one-hour general anesthesia and an overnight stay in the hospital.
You May Like: Sit N Sleep Costa Mesa
What Are The Types Of Surgical Procedures For Sleep Disorders
There are different types of surgery for sleep apnea and snoring. Surgery may be a multi-step process involving more than one procedure. You may need to continue using CPAP even when surgery successfully reduces the severity of sleep apnea. It is important to follow up regularly with your sleep doctor after surgery.
Surgical options include:
Adenoid Or Tonsil Removal
adenotonsillectomy. In this procedure, the surgeon removes the adenoids and tonsils. Removing these structures can open up the airways and improve sleep apnea.
According to a , children who are not obese and have smaller tonsils may find that recovery and risk are lower if just the adenoids get removed. However, if the tonsils are larger, the surgery may not be as effective as removing both.
Don’t Miss: Dr Barbara Sturm Sleep Food
How Does Sleep Apnea Affect Anesthesia
Anesthesia, especially general anesthesia, can be dangerous for people with obstructive sleep apnea. The condition makes anesthesia riskier because it slows down breathing and can make you more sensitive to its effects. Sleep apnea also can make it more difficult to regain consciousness and take a breath after surgery.
The condition makes anesthesia riskier because it slows down breathing and can make you more sensitive to its effects.
How Does Sleep Apnea Surgery Compare To Other Treatments
Comparing sleep apnea surgeries to other treatments is difficult. The gold standard treatment for sleep apnea is CPAP therapy. In general, healthcare professionals often prefer to try non-invasive therapies first, because of the potential risks attached to surgery.
Choosing the right surgery requires a clear understanding of what is causing symptoms, and especially in the case of OSA, this can vary from person to person. Moreover, surgical treatments may become less effective over time if people age or gain weight, which could cause sleep apnea symptoms to reappear.
Recommended Reading: Difference Between Sleep Number Beds
What Can You Do To Reduce Your Risk
If you have, or think you might have, obstructive sleep apnea, the most important thing you can do to reduce risks from anesthesia is talk to your physician or surgeon to be sure your anesthesia care is led by a physician anesthesiologist â before, during, and after surgery.
The physician anesthesiologist will discuss your symptoms and precautions that can be taken to decrease potential complications, including monitoring even more closely during and after surgery and choosing certain anesthesia medications over others. The physician anesthesiologist also will provide you with guidelines to follow in preparing for surgery.
Physician anesthesiologists work with your surgical team to evaluate, monitor, and supervise your care before, during, and after surgeryâdelivering anesthesia, leading the Anesthesia Care Team, and ensuring your optimal safety.