Central Sleep Apnea In Medical Conditions
Heart failure. Javaheri reported a prevalence of 31% for central sleep apnea in a combined sample of 5 studies with systolic heart failure . In a study of asymptomatic heart failure patients , central apnea index of 15 or more hours was seen in 55%, with a higher prevalence in ischemic versus non-ischemic cardiomyopathy . In 20 patients with symptomatic diastolic heart failure , 4 had central sleep apnea, and 2 had Cheyne-Stokes respiration .
Although heart failure is a risk factor for central sleep apnea and Cheyne-Stokes respiration, studies have failed to consistently show improved central sleep apnea or Cheyne-Stokes respiration with heart transplant. In a prospective cohort of 13 patients with heart failure and central sleep apnea, central sleep apnea improved in 7 of 13 and persisted in 3 of 13 , whereas 7 of 13 acquired obstructive sleep apnea more than 6 months after heart transplant despite normalized cardiac function and sympathetic nerve activity . Others also reported similar findings of improved central sleep apnea , persistent central apnea , and development of obstructive sleep apnea after heart transplant .
Cerebrovascular disease. According to meta-analysis of 17 studies, central sleep apnea or Cheyne-Stokes respiration was seen in 7% of patients after stroke and transient ischemic attack . Overall prevalence of central sleep apnea was 12% in stroke or transient ischemic attack in another meta-analysis .
Home Remedies For Sleep Apnea
Dr. Abhinav Singh, Sleep Physician
Fact Checked
Our dedicated team rigorously evaluates every article, guide, and product to ensure the information is accurate and factual. Learn More
Our dedicated team rigorously evaluates every article and guide to ensure the information is factual, up-to-date and free of bias.
Medical Disclaimer: The content on this page should not be taken as medical advice or used as a recommendation for any specific treatment. Always consult your doctor before taking any new medication or changing your current dosage.
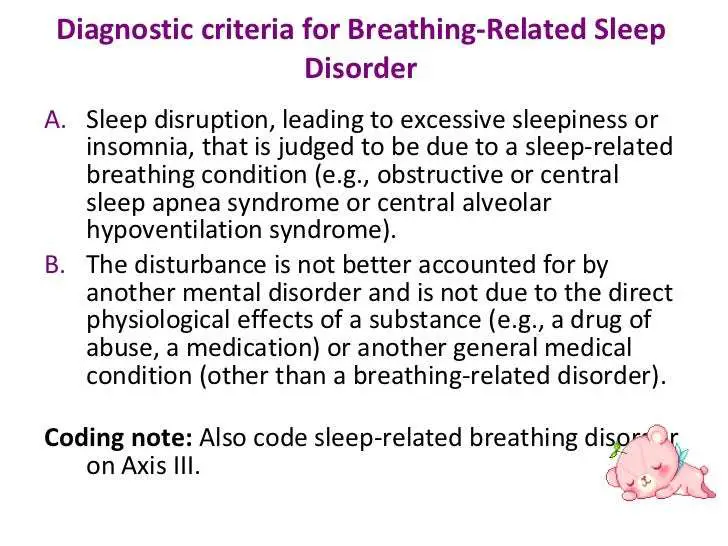
Sleep apnea is a sleep disorder in which a sleeper temporarily stops breathing throughout the night. There are two main types of sleep apnea. People with obstructive sleep apnea experience breathing pauses due to the airway briefly collapsing. Central sleep apnea involves a disconnect with how breathing is regulated in the brain. Some individuals have a combination of the two, or mixed sleep apnea.
Symptoms of sleep apnea include excessive snoring or snorting during sleep and daytime sleepiness. Some people with sleep apnea may also experience restless sleep, fatigue or grogginess in the morning, and low energy throughout the day.
Treatment of sleep apnea aims to reduce or eliminate these symptoms. It is important to treat the disorder because the resulting lack of alertness can increase the risk of accidents while driving or errors in high-risk situations. Untreated sleep apnea also raises the risk for heart problems or stroke.
Introduction To Central Sleep Apnea
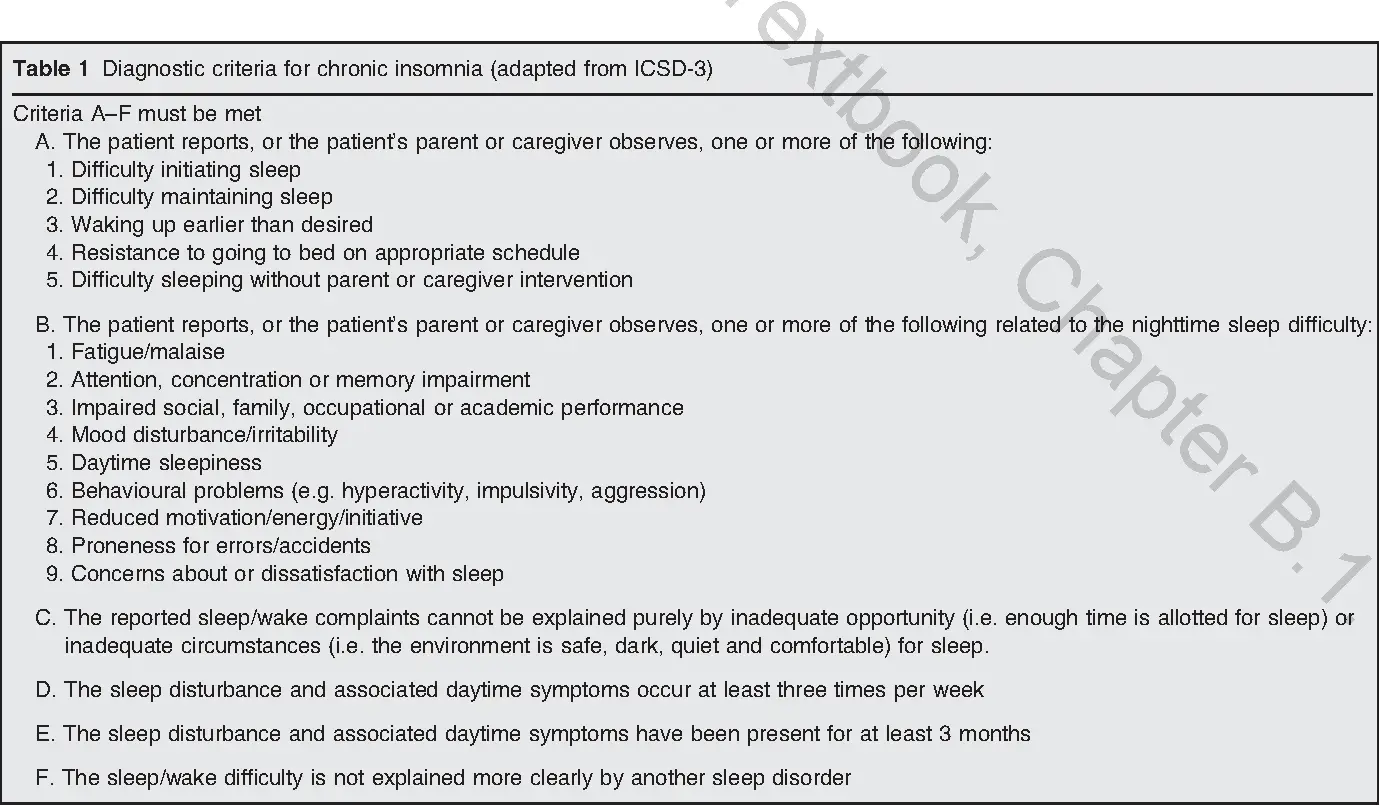
As opposed to obstructive sleep apnea , central sleep apnea is characterized by repetitive cessation of ventilation during sleep resulting from lack of ventilatory effort or drive to breathe. Whereas OSA is extremely common in the adult population, central sleep apnea affects less than 10% of patients referred to sleep laboratories. A single central apnea event is a 10-second pause in ventilation with no associated respiratory effort greater than five such events per hour are considered abnormal. CSA is present when a patient has greater than five central apneas per hour of sleep with associated symptoms of disrupted sleep . Because central apneas also may occur in an individual with obstructive apneas, clinicians may struggle to determine if CSA or OSA is the principal problem, or if a combination of the 2 disorders may need therapy.
Pearl: CSA does not have any single cause as a number of syndromes may result in CSA.
Of the causes of CSA, several are highly relevant to the cardiology community:
Pearl: Patients with Central Sleep Apnea have similar symptoms to patients with OSA, and the two disorders often co-exist.
You May Like: Why Do My Muscles Tighten Up When I Sleep
What Is The Treatment For Central Sleep Apnea
The key to treating central sleep apnea is addressing any underlying health issues that are causing the condition. The type of treatment for central sleep apnea depends on the category and subtype of central sleep apnea. For example, steps may be taken to mitigate congestive heart failure. Those on opioids or other respiratory-depression medications may gradually reduce and taper off the medications. If at high altitude, the individual can trek back to sea level. In many cases, focusing on the coexisting problem can relieve or eliminate abnormal breathing during sleep.
For many patients with central sleep apnea, the use of CPAP or BiPAP machines can decrease cessations in respiration. Supplemental oxygen may be used in a similar way.
In 2017, the Food and Drug Administration approved an implantable device that stimulates breathing-related muscles as a treatment for CSA. This treatment has shown promise in improving breathing and sleep quality in some research studies.
Depending on a persons situation, a combination of treatments may be used in order to best address their symptoms. A healthcare provider with a specialty in sleep medicine would be best to review the benefits and side effects of various treatment options for central sleep apnea.
- Was this article helpful?
Summary And Future Perspectives
Research in recent decades has improved our understanding of the various pathophysiological components underlying the different phenotypes of central breathing disturbances during sleep. They differ in terms of increased or dampened respiratory drive but also in comorbidities and underlying diseases. Proceedings of medical therapy have led to new clinical phenomena, such as opioid-induced CSA or treatment-emergent CSA. It has become obvious that a precise description of the polysomnographic pattern on the one hand and the clinical situation on the other hand is crucial. However, due to a lack of sufficient evidence, several questions on the impact of central breathing disturbances during sleep and optimal treatment remain open, including:
1) prognostic relevance of CSA
2) indication for treatment of CSA
3) differential therapy based on pathophysiological components and
4) long-term efficacy of PAP therapies and long-term outcome of untreated patients with different phenotypes.
Also Check: How To Sleep When You Have Whiplash
What Is The Apnea
The apnea-hypopnea index is a diagnostic tool for determining the presence and severity of obstructive sleep apnea .
People with OSA experience a collapse of their airways during sleep. When this causes their breathing to completely stop or reduce to 10% of normal levels for at least 10 seconds, it is called an apnea. Hypopneas occur when your airways partially collapse, resulting in shallow breathing. If your airflow decreases by more than 30% for at least 10 seconds, it can be considered a hypopnea. Apneic and hypopneic events disrupt sleep and lead to lower blood oxygen levels, contributing to long-term health complications.
The AHI sleep apnea scale helps doctors calculate the severity of your symptoms. The AHI is different from the central apnea-central hypopnea index used for central sleep apnea, a form of sleep apnea that develops when the brain fails to tell the respiratory muscles to breathe.
Deterrence And Patient Education
The patients and families need to understand the physiology and mechanism causing sleep apnea. During regular sleep, the air can move through the respiratory tract at a normal rhythm. Still, there is the transient cessation of air movement with resultant reduction in breathing in patients with central sleep apnea because of breathing control and rhythm changes. Central sleep apnea has a long-term impact on health and quality of life. Symptoms may include restless sleep, low energy, difficulty concentrating, memory impairment, and waking up unrested.
The goal standard for diagnosis is a sleep study called polysomnogram that measures breathing effort and airflow, vitals, and blood oxygen level during different stages of sleep. Treatment includes identifying underlying causes and treating any precipitating factors. Ideally, these patients need to be evaluated by a sleep physician.
Don’t Miss: Sit N Sleep Customer Service
Discuss Medication Side Effects With Your Doctor
If you are currently taking medication to address other health concerns, your doctor should closely monitor your treatment plan. It is important to tell your doctor if you believe your current medications are worsening your sleep apnea symptoms. They will be able to assess your current treatments, evaluate your dosage, and consider alternatives.
Certain types of medications that cause drowsiness and slow brain activity may worsen sleep apnea symptoms.
How To Properly Score Each Type Of Apnea
The distinction between central and obstructive hypopneas got lost somewhere along the line, and labs started to score and report them as a single entity. This has changed.
The goal of a sleep professional is to treat your patients and ensure their breathing patterns are stabilized. For you to do this, you have to have the proper equipment. Where CPAP works well for obstructive apneas and hypopnea events, other treatment modalities work better for most central events. Central apnea episodes are typically better controlled with either Bi-level pressure support or additional backup support through a Bi-level ST.
But, central hypopneas aren’t always controlled by any of these devices. For a more complex case of central hypopnea, you’ll have to give your patients Adaptive Servo Ventilation which is a more advanced therapy.
If you don’t know the difference between central and obstructive hypopneas, you’ll find it difficult to determine which device is best suited for the job.
Your patients that have complex breathing patterns might not have central apneas but may have central hypopneas involved in the waxing and waning pattern of breathing. When you don’t have enough documentation on central events, it can be difficult to obtain insurance coverage.
Recommended Reading: Sleep Number Flexfit 2 Dimensions
How To Treat Central Sleep Apnea
PAP is the treatment most often used for CSA. It is delivered through a mask that you wear over the nose alone or the nose and mouth. The air gently blows into the back of the throat. This keeps the airway open so you can keep breathing as you sleep.
The amount of air pressure needed is different for each person. A CPAP study will show what level is right for you. Often a variation of PAP, called BPAP , is used.
A thorough evaluation and treatment of underlying medical conditions needs to be done. Heart failure or kidney failure needs specific treatment. Stroke may require special care such as rehabilitation and a careful assessment of your risk of having another stroke.
In the case of high-altitude periodic breathing, no specific treatment may be needed but other problems that occur at high altitudes may need to be addressed. Some of these may respond to medication. Others require avoiding high altitudes and are often reversible by descending to a lower altitude.
In the case of CSA due to drug or substance, a change of medication or discontinuation of the medication or substance may be needed.
Some patients with CSA may be treated with upper airway stimulation. The implanted device stimulates the nerve that sends signals to the diaphragm to stimulate breathing.
Central Vs Obstructive Sleep Apnea
Sleep apnea is when someone repeatedly stops breathing while they are sleeping.1 Breathing stops temporarily and then recommences, causing sudden drops in blood oxygen levels. Sleep apnea symptoms include a dry mouth upon waking, insomnia, daytime grogginess, and irritability.2
There are three types of sleep apnea. Central sleep apnea is when the sleep apnea cause is due to the actual central nervous signals for breathing. Breathing may also be halted by the relaxation of throat muscles, known as obstructive sleep apnea. When both occur, the condition is known as complex sleep apnea syndrome. There are different risk factors, complications, and treatments for central vs obstructive sleep apnea, so it is important to identify which type is afflicting a patient.
Don’t Miss: What Is The Best Sleep Number Bed
How Is Ahi Measured
The apnea-hypopnea index represents the average number of apneas and hypopneas you experience each hour during sleep. To measure it, doctors divide the total number of apneic and hypopneic events by the total number of hours you were asleep. To register as an event, an apnea or hypopnea must last at least 10 seconds or longer.
Doctors typically calculate AHI during a sleep study, or polysomnogram, which monitors your brain waves, blood oxygen levels, heart rate, and breathing while you sleep. Polysomnography generally takes place at a sleep laboratory, but some may be able to perform a simplified version at home.
While the AHI is the primary measurement for diagnosing OSA, your doctor may review other metrics to better understand the severity of your OSA. For example, the oxygen desaturation index measures how many times per hour, on average, your blood oxygen levels fall below normal for 10 seconds or longer. Another important metric, especially for children, is the level of carbon dioxide in the blood. A high level of carbon dioxide may arise due to a long period of breathing at less than full capacity, even if the airway is not completely blocked.
Csa Due To Medication
Drugs in common use for pain control include morphine, fentanyl and methadone. Patients on high doses of these medications may have a slow sleeping respiratory rate. They may develop long obstructive apnoeas. Ataxic breathing is commonly observed with variation in respiratory rate and tidal volume. Relatively few arousals are noted and stage N3 can be increased. Periodic breathing and intermittent central apnoeas are seen and these may even occur in stage N3. Treatment emergent central apnoeas are also common even if the diagnostic study might have shown mainly obstructive events. Reduction in opiate dose is a logical first step if this were possible. Patients with mostly obstructive events respond to CPAP but then central apnoeas may emerge or persist . Javaheri et al. reported on ASV being effective treatment for both central and obstructive apnoea in opiate induced complex SA . It is essential to increase EPAP sufficiently to eliminate upper airway obstructive events in these situations.
Read Also: Sleep Number P5 King Bed Reviews
Congenital Central Hypoventilation Syndrome
Congenital central hypoventilation syndrome , often referred to by its older name “Ondine’s curse,” is a rare and very severe inborn form of abnormal interruption and reduction in breathing during sleep. This condition involves a specific homeobox gene, PHOX2B, which guides maturation of the autonomic nervous system certain loss-of-function mutations interfere with the brain’s development of the ability to effectively control breathing. There may be a recognizable pattern of facial features among individuals affected with this syndrome.
Once almost uniformly fatal, CCHS is now treatable. Children who have it must have tracheotomies and access to mechanical ventilation on respirators while sleeping, but most do not need to use a respirator while awake. The use of a diaphragmatic pacemaker may offer an alternative for some patients. When pacemakers have enabled some children to sleep without the use of a mechanical respirator, reported cases still required the tracheotomy to remain in place because the vocal cords did not move apart with inhalation.
Persons with the syndrome who survive to adulthood are strongly instructed to avoid certain condition-aggravating factors, such as alcohol use, which can easily prove lethal.
Central Sleep Apnea Causes And Types
There are several types of central sleep apnea, each with a different cause.
- Cheyne-Stokes breathing. This is when your breathing speeds up, slows down, stops, and then starts again. Each of these cycles can last 30 seconds to 2 minutes. Cheyne-Stokes breathing is common in people whove had heart failure or a stroke. It happens in about half of central sleep apnea cases.
- Narcotic-induced central sleep apnea.Opioid medications like morphine, oxycodone, and codeine can affect your breathing patterns.
- High-altitude periodic breathing. Many people have trouble breathing when they go up to a high elevation, usually 2,500 meters or more.
- Treatment-emergent apnea. About 5% to 15% of people who have positive airway pressure treatment for obstructive sleep apnea get CSA.
- Medical condition-induced apnea. Health problems like heart failure, Parkinsons disease, stroke, and kidney failure can cause CSA.
- Idiopathic central sleep apnea. This is when theres no clear cause.
A related condition named congenital central hypoventilation syndrome is linked to a certain gene. It affects about one in 200,000 children around the world.
Continued
Recommended Reading: Sleep Number I8 Vs I10 Reviews
How Common Is Central Sleep Apnea
While the exact number of people with central sleep apnea is unknown, it is estimated that about .9% of people over 40 in the United States have the condition. Though it affects both men and women, it occurs more often in men of greater than 65 years old. People who have a heart condition, use narcotics, suffer from a stroke, live in high altitudes, or use CPAP are at greater risk for central sleep apnea.
Csa In Other Internal Or Neurological Diseases Other Than Cardiovascular Diseases
2.5.1. CSA in other internal diseases
Certain endocrine diseases have been reported to be associated with CSA. No systematic screening efforts are performed today with the exception of screening procedures for OSA in acromegaly patients.
Acromegaly
SDB is frequent in patients with acromegaly and the majority of these patients present with OSA. A number of studies has reported an increased prevalence of CSA of up to 32% , but more recent studies could not confirm those findings . In total, close to 10% of patients with acromegaly fulfil the criteria for CSA, which may be considered as mild CSA. The central apnoea index was associated with serum levels of growth hormone, and increased ventilatory responses were associated with growth hormone and insulin-like growth factor-1 levels, suggesting specific pathogenic mechanisms explaining the occurrence of CSA in acromegaly . In addition, patients with CSA also have concomitant cardiac diseases . Surgical or medical treatment of acromegaly may reduce OSA. However, there are no controlled studies addressing treatment effects on CSA .
Diabetes mellitus
End-stage renal disease
OSA is frequent in end-stage renal disease . Tadaet al. reported on 30 patients with sleep apnoea in a group of 78 patients on haemodialysis. However, the mean CAI was 4.1 events per h and central apnoea constituted 8% of all SDB events. Eight out of 30 patients showed an elevated CAI and were subsequently classified as patients with CSA.
Statements
Statements
Recommended Reading: Plywood For Sleep Number Bed