Due To Drug Or Substance
This breathing pattern can vary from a regular increasing and decreasing respiratory effort to something that is quite irregular. Sometimes there are elements of obstruction such as the breathing that is seen in OSA. Medications most associated with this central sleep apnea pattern are in the opioid category such as prescription pain medications or illicit substances such as heroin.
What Happens When You Stop Breathing
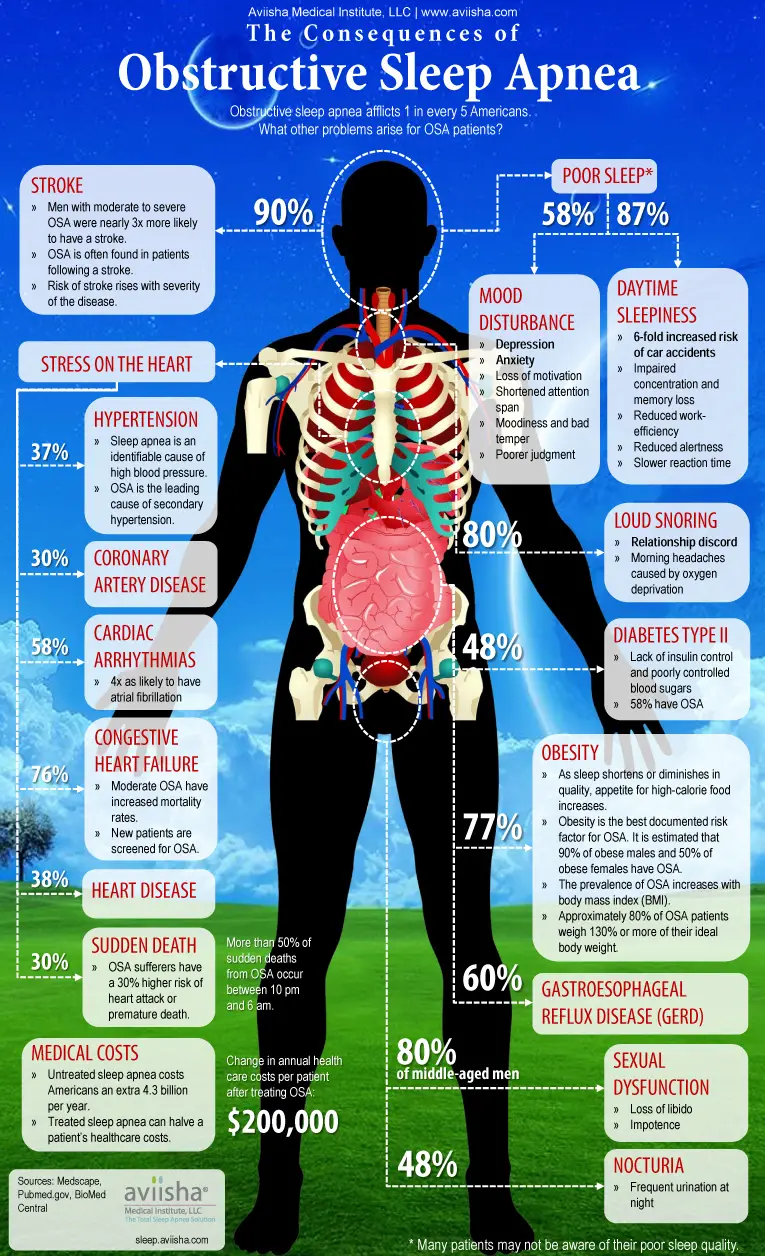
When you stop breathing, your heart rate also tends to drop the longer your body is deprived of oxygen. Then, your involuntary reflexes cause you to startle awake at the end of that period of not breathing. When this occurs, your heart rate tends to accelerate quickly and your blood pressure rises.
These are changes that take place acutely when you stop breathing. However, your body starts to experience chronic effects if you experience frequent apnea. Data suggests increased risk, particularly when you stop breathing roughly 30 times or more per hour. But there is likely a risk at even lower frequency rates.
For example, your blood pressure tends to go up, your heart walls thicken due to increased workload and the structure of your heart changes. It tends to become stiffer and less flexible because there are more fibrous cells growing in between the muscle cells.
All of those things increase the risk that you can have either atrial or ventricular arrhythmias. They also tend to reduce the function of the heart so that its less efficient at pumping blood.
Sleep Apnoea Can Cause Other Problems
Without treatment, sleep apnoea can lead to:
- a higher chance of having a stroke
- depression or changes in your mood
- a higher chance of having a serious accident caused by tiredness, such as a car accident
- difficulty concentrating at work or school
Sleep apnoea can also be difficult for your partner and put a strain on your relationship with them.
Read Also: Does The Garmin Vivofit 4 Track Sleep
You May Like: Sleep Train Vs Mattress Firm
Implantable Phrenic Nerve Stimulation
Phrenic Nerve Stimulation is an FDA-approved, implantable, non-mask therapy for moderate to severe central sleep apnea in adult patients. The device activates automatically each night to send signals to the breathing muscle via the phrenic nerve to restore a normal breathing pattern. It monitors respiratory signals while you sleep and helps restore normal breathing patterns. Because the device is implantable and activates automatically, it does not require wearing a mask however, as with any implantable device procedure, there is a risk of implant site infection.12
Positive Airway Pressure THERAPY
Positive airway pressure devices are often used to treat central sleep apnea. Various types exist, including those that provide continuous pressure and those that provide variable pressure . Notably, ASV, or adaptive-servo ventilation, is contraindicated in patients with chronic, symptomatic heart failure with reduced left ventricular ejection fraction .11
Supplemental Oxygen
Physicians may recommend the use of supplemental oxygen for patients with central sleep apnea. Various options can be used to deliver oxygen to the patient.13
Pharmacological
Pharmacological agents such as acetazolamide and theophylline have been attempted as therapies for central sleep apnea. However, limited data has been collected for the efficacy and safety of these therapies.
Central Sleep Apnea Happens When The Brain Is Involved

Central sleep apnea is less common than obstructive sleep apnea. It can also be trickier to diagnose and treat. Unlike obstructive sleep apnea, which is caused by a mechanical problem that blocks the airway, central sleep apnea occurs because the brain is not sending the proper messages to the muscles that control breathing. Central sleep apnea is caused by a neurological reason, explains Dr. Capasso.
Recommended Reading: Sleep Number Bed Vs Tempurpedic Reviews
What Is The Worst Sleep Position For Sleep Apnea
The worst sleep position for Sleep Apnea is sleeping on your back. When you are in this position, it causes the airway to collapse and make breathing difficult. This can also lead to snoring since the tongue falls backward blocking off your throat which makes any sound that may come out of our nose become muffled or silenced completely. If you have been diagnosed with sleep apnea then its important to be aware of what kind of positions help alleviate these symptoms as well as being mindful about not going into them during those times when we feel exhausted or sleepy.
How To Properly Score Each Type Of Apnea
The distinction between central and obstructive hypopneas got lost somewhere along the line, and labs started to score and report them as a single entity. This has changed.
The goal of a sleep professional is to treat your patients and ensure their breathing patterns are stabilized. For you to do this, you have to have the proper equipment. Where CPAP works well for obstructive apneas and hypopnea events, other treatment modalities work better for most central events. Central apnea episodes are typically better controlled with either Bi-level pressure support or additional backup support through a Bi-level ST.
But, central hypopneas aren’t always controlled by any of these devices. For a more complex case of central hypopnea, you’ll have to give your patients Adaptive Servo Ventilation which is a more advanced therapy.
If you don’t know the difference between central and obstructive hypopneas, you’ll find it difficult to determine which device is best suited for the job.
Your patients that have complex breathing patterns might not have central apneas but may have central hypopneas involved in the waxing and waning pattern of breathing. When you don’t have enough documentation on central events, it can be difficult to obtain insurance coverage.
Read Also: Lasik Eye Surgery Do They Put You To Sleep
Causes Of Central Sleep Apnea
As discussed above, the main cause of CSA is a misfire in communication from the brain stem to the respiratory system. There is another cause why central sleep apnea is on the rise and may just relate to the growing epidemic of opiate use in the United States.
Opioid use Can Cause Central Sleep Apnea
According to the United States National Library of Medicine, 8 clinical studies were done in order to relate opioid use to central sleep apnea. The results of the study showed that 24% of chronic opioid users have central sleep apnea. It was also found that most opioid users had a very low body mass index. If you are prescribed opioids, its possible that you could develop central sleep apnea since opioids target receptors in the brain. If you endure extreme pain, opioids are generally described to block pain and generally calm the body. This calming can actually overact, stopping the brain stem from sensing the amount of oxygen in the blood and not triggering your respiratory system to function.
Snoring is not as prominent in CSA
Unlike obstructive sleep apnea, snoring isnt as prevalent in CSA because the brain is not signaling breathing from occurring, as opposed to a physical obstruction in airflow like in OSA.
Snoring: A Big Red Flag
See the snoring help section below on how to get rid of snoring.
Another one of the major characteristics people typically have is high decibel, vacuum-cleaner-noise-levelsnoring.Does your partner snore like a leaf blower and rattle the walls with their snoring? Is their snoring intermittent or cyclic , with frequent periods of silence?
Or are you a snorer whose bed partner has had to escape to another part of the house in order to get a good night’s sleep…because you snore like a freight train?
If so, consider these as important warning signs that something is not right. Apnea is associated with snoring and snoring is a sign of impaired breathing. However, just because someone snores does not mean they have this disorder. But if the snoring is really loud, beware!
Especially beware if you have two of the other killer sleep apnea symptoms sufferers usually have:
Don’t Miss: Flexfit 3 Sleep Number Bed
Two Types Of Sleep Apnea: Obstructive And Central
July 22, 2020// by Terry Cralle//
Sleep apnea is a type of sleep disorder that occurs when a person experience pauses in breathing during sleep. In cases of untreated sleep apnea, people experience a complete halt in breathing for several seconds, repeatedly during sleep. This can be potentially dangerous and sleep apnea is considered a serious disorder.
Sleep apnea can affect people of all ages, but it is most common with people over the age of 40 and people who are overweight. This condition also occurs in approximately 25% of men and 10% of women. There are, of course, certain risk factors for sleep apnea, which increase ones chance of developing the condition. Luckily, sleep apnea can be treated with CPAP, BiPAP, or APAP machine therapy, mouthpieces, medicaments, or surgery.
In the following paragraphs, were going to take a look at the types of sleep apnea that people can develop. Well see what the similarities and differences between these types are and how theyre treated. So, without further ado, lets get started!
How Is Central Sleep Apnea Diagnosed
A definitive diagnosis of CSA is made using an in-lab polysomnography, which is a detailed sleep study that measures breathing, respiratory effort, electrocardiogram, heart rate, oxygen, eye movement activity, muscle activity, and electrical activity of the brain during an overnight stay in a sleep clinic.
Because central sleep apnea can be tied to several health problems, a healthcare provider may also recommend other tests, such as a brain scan or an echocardiogram of the heart to determine the underlying cause.
Anyone who has noticed potential symptoms of central sleep apnea should speak with a doctor who can review their situation and determine if any diagnostic testing is appropriate.
Don’t Miss: Stomach Sleeper Memory Foam Mattress
Accepting New Patients Near Chicago Il Nationwide & Worldwide
The dangers of sleep apnea and heavy snoring are often overlooked and left untreated. Our dentists educate patients on the serious health risks that accompany obstructive sleep apnea.
Patients with apnea may awaken from 5 to more than 10 times per hour and not be aware of waking, but suffer the effects.
Read Also: Sleep App Gear S2
What Are Opioids
These are pain-relieving medications commonly taken by people with chronic conditions like cancer, or who experience acute pain following an operation or injury.
The most common forms of legal opioids are:2
- Morphine
The most common forms of illegal opioids are:2
- Heroin
- Illegally made and distributed fentanyl
Recommended Reading: Best Position To Sleep On Adjustable Bed
What Can You Do
Many people with sleep apnea are overweight or obese, so losing weight will improve your overall health. Quitting smoking, exercising regularly, and lowering your alcohol consumption will also help. We also recommend avoiding sedatives and sleeping pills, and trying a new sleep position to breathe better.
If you think you have sleep apnea, dont let it go untreated. Make an appointment to see Dr. Kumra by using our convenient online booking tool or by calling 646-859-6136 today.
You Might Also Enjoy
What Causes Central Sleep Apnea
CSA is often considered more dangerous than OSA because the root of the problem is in the brain. Patients with CSA have no control over their brain functions and responses, so this type of apnea is much more complicated. Central apneas occur when the brain fails to adequately support the bodys respiratory system it doesnt respond to the systems needs.
- Poor Brain-Breath Communication:
- Brain Malfunction: During an episode of CSA, the brain does not respond to carbon dioxide and blood level changes in the body quickly enough. Essentially, the centers of the brain that help us to breathe are not working to keep blood and carbon dioxide levels balanced and the body stops breathing.
- Respiratory Response: The respiratory system only breathes when it receives messages from the brain telling it to do so. If the brain is not registering unhealthy levels of blood and carbon dioxide in the body, it is not telling the body to breathe and balance out the levels. Patients with OSA attempt to breathe but are not successful. Patients with CSA, however, make no attempt to breathe because they have not received instructions from the brain. During CSA, the entire respiratory system stops functioning.
Read Also: Sleep Number Bed Help With Snoring
Sleep Apnoea Can Affect Your Driving Ability
People with significant sleep apnoea have an increased risk of motor vehicle accidents. Driving authorities recognise certain sleep disorders, including sleep apnoea that can affect driving fitness.
If you live in Victoria, you are legally required to notify VicRoads of any serious or chronic medical condition, injury or disability or the effects of certain treatments that may affect your ability to drive. Failure to do so may affect your insurance cover.
People with sleep apnoea will be assessed on a case-by-case basis and you may be advised to provide medical reports on the severity and treatment of your sleep apnoea. Options may include the issue of a conditional licence until your sleep apnoea is adequately treated.
People with sleep apnoea should also be aware of safety in other situations in which falling asleep could pose a danger to other people.
Central Sleep Apnea Causes And Associations
Central sleep apnea is caused by a failure of a persons brain to consistently send signals to activate the breathing muscles while asleep. Central sleep apnea has a number of known associations, including2
- Cardiac disorders, including congestive heart failure and atrial fibrillation
- High altitude
- Treatment emergent central sleep apnea
- Idiopathic central sleep apnea
- Other medical conditions
CARDIAC DISORDERS
Studies have shown that up to 40% of people with congestive heart failure and 30% of people with atrial fibrillation may have central sleep apnea.10,11 In fact, heart failure is the most common cause of CSA in the general population.2
HIGH ALTITUDE
Periodic breathing appears when people are exposed to high altitudes. This may be due to how your body responds to changes in the atmosphere.2
OPIOIDS
Certain medications, including opioids, can disrupt the breathing pattern and lead to central sleep apnea.2
TREATMENT EMERGENT CENTRAL SLEEP APNEA
Treatment emergent central sleep apnea refers to central events that occur when a person is using Positive Airway Pressure therapy such as CPAP or BiPAP. Reasons for treatment emergent CSA may occur due to an increased number of arousals during titration, mask leak, or overtitration. This may improve with ongoing PAP use.2
IDIOPATHIC CENTRAL SLEEP APNEA
Don’t Miss: Nest Bedding Love And Sleep
P Stands For Pressure High Blood Pressure
Obstructive sleep apnea can lead to hypertension. Every time a person stops breathing for a few seconds, the bodys sympathetic nervous system goes into action and raises blood pressure. In addition, the body releases stress hormones called catecholamines, which can also raise blood pressure over time.
While having hypertension by itself is not a sign of a sleep disorder, it can be a warning sign when combined with other telltale signals. Fortunately, treatments for obstructive sleep apnea, like continuous positive airway pressure, or CPAP, have not only been shown to help with sleep apnea, but they also lower blood pressure.
What Can Cause Central Sleep Apnea
There are six different types of central sleep apnea that are differentiated by their cause.
- Medical Condition-Induced Apnea CSA can be caused by brain damage from an injury or encephalitis affecting the lower brainstem, the area of the brain responsible for breathing. It can also be caused other serious illnesses, particularly Parkinsons disease, Alzheimers, ALS, hypothyroidism, and chronic kidney disease.
- Cheyne-Stokes breathing People affected by this type of CSA have an irregular breathing cycle in which respiration speeds up, slows down, then stops and restarts. The pattern can last between 30 seconds and two minutes. This kind of CSA and is often seen in patients who have had a stroke or heart failure.
- Treatment-Emergent Apnea About 5% to 15% of people using CPAP therapy for obstructive sleep apnea develop CSA.
- Narcotic-Induced CSA This refers to disordered breathing caused by opioid medications.
- High-Altitude Periodic Breathing Many people at high elevations above 2,500 meters .
- Idiopathic CSA Describes central sleep apnea that cannot be traced to a clear cause.
Recommended Reading: Best Price On Sleep Number Bed
More Sleep Apnea Symptoms
Now that I’ve given you four of the main sleep apnea symptoms to look for, let me close this article by giving you the full list of all the symptoms sleep apnea is associated with:
The symptoms sleep apnea produces are some of the most undiagnosed conditions in medicine and may often go undetected by your local doctor. So by you knowing what signs to look for, you are better equipped to do something about this serious sleep disorder.
And if you or someone you love has these sleep apnea symptoms, you probably want to know “What is sleep apnea anyway?” See my article on that in the more helpful articles section below.
How To Diagnose Central Sleep Apnea

Sleep doctors have training and expertise in this area. The doctor will review your medical history and symptoms. In the case of high-altitude periodic breathing, the detailed history alone should be enough to detect the problem. If needed, the doctor will schedule you for a sleep study.
Most of the causes of CSA are serious conditions that should be evaluated and treated. A sleep doctor can put together a treatment plan just for you. First, she must evaluate the causes of CSA and look for other conditions that create similar problems with sleeping. These include the following:
- Another sleep disorder
- A mental health disorder
- Substance abuse
The doctor will need to know your symptoms and how long you have had them. She will also want to know if your symptoms began at the same time as other medical problems or when you slept at a high altitude.
Get information from those who sleep with you or have seen you sleep. This includes spouses, relatives, friends, teammates, and roommates. You will also need to provide a complete medical history.
Keep a sleep diary for two weeks. Include the following information:
- What time you went to bed each night
- What time you got up in the morning
- How many times you woke up during the night
- Whether you felt rested when you woke up
- If you took naps during the day
- Whether you felt sleepy or rested throughout the day
You May Like: How To Lose Weight Fast While Sleeping